Pyeloplasty is a type of reconstructive surgery used to correct conditions affecting the renal pelvis and ureter, typically aimed at treating an obstruction known as ureteropelvic junction (UPJ) obstruction. This surgical procedure plays a crucial role in alleviating conditions that prevent proper urine flow from the kidney to the bladder, which can lead to kidney damage over time if left untreated. Pyeloplasty can be performed using various surgical techniques, and one of the advanced approaches involves using different types of “flaps” to achieve optimal results. These flap techniques in pyeloplasty are particularly beneficial in complicated cases where conventional methods might not yield satisfactory results pyeloplasty flapsa.
This article aims to provide a comprehensive overview of pyeloplasty and the different flap techniques used in this surgical procedure. We will explore the causes, symptoms, and diagnosis of UPJ obstruction, explain the types of pyeloplasty surgeries, examine various flap techniques, and discuss the benefits, risks, and postoperative considerations associated with this surgery.
1. What is Pyeloplasty?
Pyeloplasty is a surgical procedure primarily used to relieve obstructions at the ureteropelvic junction (UPJ), which is the point where the ureter (the tube that carries urine from the kidney to the bladder) meets the renal pelvis (the funnel-like part of the kidney where urine collects). An obstruction at the UPJ can lead to a condition called hydronephrosis, where urine backs up in the kidney, causing swelling and potentially damaging kidney tissue.
The goal of pyeloplasty is to remove the blockage and restore the free flow of urine, thus relieving symptoms and preserving kidney function. This procedure is commonly performed in both children and adults, as UPJ obstruction can be a congenital condition or develop over time due to scarring, trauma, or kidney stones.
2. Causes and Symptoms of Ureteropelvic Junction Obstruction
Causes
UPJ obstruction may have various underlying causes, including:
- Congenital abnormalities: Some people are born with a narrowing of the UPJ, which causes a partial or complete blockage. This is the most common cause in children.
- Scar tissue: Injury, infection, or previous surgeries involving the urinary tract can lead to the formation of scar tissue, which may obstruct the UPJ.
- Kidney stones: Stones in the renal pelvis or ureter can obstruct the flow of urine.
- Blood vessels: In some cases, blood vessels near the UPJ can compress the ureter, leading to an obstruction.
Symptoms
Symptoms of UPJ obstruction may vary depending on the severity of the blockage and the age of the patient. Common symptoms include:
- Pain: Dull, aching pain in the flank or back is often associated with UPJ obstruction, especially after consuming large amounts of fluid.
- Nausea and vomiting: When the blockage is severe, patients may experience gastrointestinal symptoms.
- Recurrent urinary tract infections: UPJ obstruction can make the urinary system more prone to infections.
- Hematuria (blood in urine): This may occur due to irritation or injury to the kidney.
- Decreased kidney function: In severe cases, UPJ obstruction can lead to a decline in kidney function, which may be detected through routine blood tests.
3. Diagnosis of UPJ Obstruction
Diagnosing UPJ obstruction typically involves a combination of medical history, physical examination, and imaging studies. Key diagnostic tools include:
- Ultrasound: Often the first imaging test used, ultrasound can reveal swelling of the kidney (hydronephrosis) and suggest an obstruction.
- CT Scan: Provides more detailed images, which can help pinpoint the location and severity of the blockage.
- Nuclear Renal Scan: Measures kidney function and assesses how well urine is draining from the kidney.
- Intravenous Pyelogram (IVP): A type of X-ray that uses contrast dye to visualize the urinary tract.
- Retrograde Pyelography: Involves inserting contrast dye directly into the ureter through a cystoscope to provide detailed images of the UPJ area.
Once the diagnosis is confirmed, the next step is to determine the most suitable surgical approach, which often includes evaluating whether a traditional pyeloplasty or a flap technique is needed.
4. Types of Pyeloplasty Procedures
There are several surgical approaches to pyeloplasty, each with specific advantages depending on the patient’s condition and the surgeon’s preference. Here are the main types:
a. Open Pyeloplasty
Open pyeloplasty is a traditional surgical approach that involves making a large incision in the flank or abdomen to access the kidney and ureter. The surgeon removes the obstruction and reconstructs the UPJ. While effective, open pyeloplasty has a longer recovery time and may leave a visible scar.
b. Laparoscopic Pyeloplasty
Laparoscopic pyeloplasty is a minimally invasive alternative that involves small incisions and the use of a laparoscope (a thin tube with a camera). This approach results in less postoperative pain, quicker recovery, and minimal scarring. Laparoscopic pyeloplasty has a high success rate, similar to open surgery, and is becoming increasingly popular.
c. Robotic-Assisted Pyeloplasty
Robotic-assisted pyeloplasty is a modern, minimally invasive approach that uses robotic arms controlled by the surgeon. The precision of robotic surgery is especially useful in complex cases, as it allows for greater dexterity and control. This technique is often favored for patients with difficult anatomy or complex UPJ obstructions.
d. Endopyelotomy
Endopyelotomy is a less invasive technique in which an incision is made internally at the UPJ using a specialized instrument or laser. Although this procedure can be effective for certain patients, the success rate is generally lower than with pyeloplasty, and it may not be suitable for severe obstructions or complex cases.
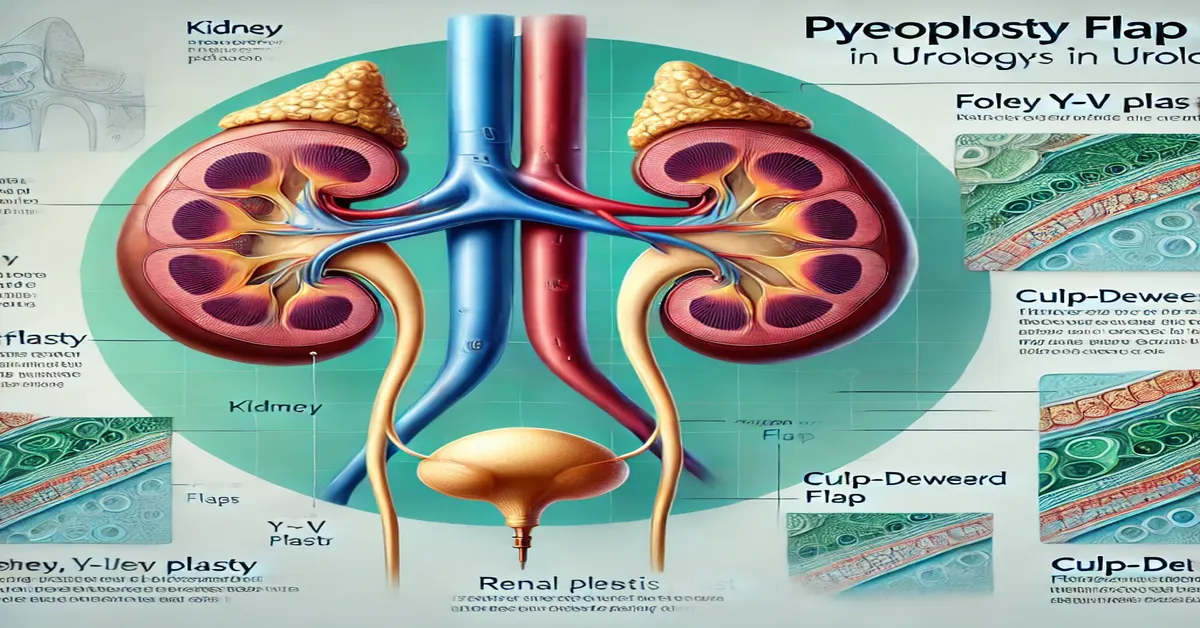
5. Flap Techniques in Pyeloplasty
In cases where conventional pyeloplasty techniques are insufficient, flap techniques may be employed to create a larger and more functional connection between the renal pelvis and ureter. Flap techniques involve creating a “flap” of tissue from the renal pelvis or ureter and using it to reconstruct the UPJ. This approach is particularly useful in cases where the ureter is narrow or damaged, or when there is a need to preserve as much healthy tissue as possible pyeloplasty flapsa.
a. Culp-DeWeerd Flap
The Culp-DeWeerd flap is a commonly used technique in reconstructive urology. In this procedure, a flap is created from the renal pelvis and folded down to widen the UPJ, creating a larger and smoother pathway for urine. This technique is especially beneficial in cases with high-insertion UPJ obstructions.
b. Foley Y-V Plasty
The Foley Y-V plasty involves creating a Y-shaped incision in the renal pelvis, which is then converted into a V shape by folding and suturing the tissue. This method is particularly effective for correcting obstructions caused by scarring or narrowing of the UPJ. Foley Y-V plasty provides a broader connection between the renal pelvis and ureter, reducing the risk of re-obstruction.
c. Spiral Flap Technique
The spiral flap technique is a complex but effective procedure that involves creating a spiral-shaped flap from the renal pelvis or ureter to reconstruct the UPJ. This method is often used when there is significant narrowing of the ureter or in cases where previous surgeries have failed. The spiral flap allows for a wide and flexible passage for urine, improving long-term outcomes pyeloplasty flapsa.
d. Intubated Ureteral Stent and Flap Pyeloplasty
In some cases, a stent is used in conjunction with a flap technique to maintain the newly created opening and ensure proper healing. The stent remains in place for a few weeks after surgery and is then removed once healing is complete. This approach helps prevent postoperative complications such as stricture formation or re-obstruction.
6. Benefits and Risks of Flap Techniques in Pyeloplasty
Benefits
- Improved drainage: Flap techniques create a larger, more functional connection between the renal pelvis and ureter, enhancing urine flow.
- Reduced risk of re-obstruction: By creating a wider passage, these techniques decrease the likelihood of future blockages.
- Preservation of kidney function: Successful pyeloplasty can prevent long-term kidney damage by restoring normal urine flow.
- Minimally invasive options available: Many flap techniques can be performed laparoscopically or with robotic assistance, leading to faster recovery and less postoperative pain.
Risks
- Infection: As with any surgery, there is a risk of infection, which can typically be managed with antibiotics.
- Bleeding: While rare, bleeding may occur during or after the procedure, necessitating additional interventions.
- Stricture formation: In some cases, scar tissue can form at the site of the repair, leading to a narrowing or re-obstruction.
- Leakage: There is a risk of urine leakage from the surgical site, which may require additional treatment.
- Anesthesia-related complications: As with any surgery that requires anesthesia, there is a small risk of complications related to the use of anesthesia pyeloplasty flapsa.
7. Recovery and Postoperative Care
Following pyeloplasty, most patients can expect a recovery period that may vary depending on the type of surgery performed. Key aspects of postoperative care include:
- Hospital stay: Open pyeloplasty may require a hospital stay of several days, while laparoscopic and robotic-assisted techniques often allow for same-day or overnight discharge.
- Pain management: Patients may experience some pain at the incision site, which can be managed with prescribed pain medication.
- Stent removal: If a stent was placed during surgery, it is typically removed a few weeks postoperatively.
- Follow-up imaging: Doctors may order follow-up imaging, such as an ultrasound or nuclear scan, to ensure the kidney is draining properly.
- Activity restrictions: Patients are usually advised to avoid strenuous activity for several weeks to promote healing pyeloplasty flapsa.
- Hydration: Staying well-hydrated is crucial for optimal recovery and kidney function.
Most patients recover fully within six weeks, although it may take longer for those who undergo open surgery or have complex cases pyeloplasty flapsa.
Conclusion
Pyeloplasty is an effective surgical solution for treating UPJ obstruction, a condition that can lead to kidney damage if left untreated. The various surgical techniques available, including flap techniques, offer tailored approaches to address different complexities of UPJ obstructions. Flap techniques in pyeloplasty, such as the Culp-DeWeerd flap, Foley Y-V plasty, and spiral flap, provide enhanced outcomes in complex or recurrent cases. These advanced techniques help improve urine flow, reduce the risk of re-obstruction, and preserve kidney function.
With advances in minimally invasive and robotic-assisted approaches, pyeloplasty has become more effective, with faster recovery and lower complication rates. Understanding the options and implications of each technique can help patients and their families make informed decisions about their treatment pyeloplasty flapsa.
FAQs
- What is pyeloplasty, and why is it performed?
Pyeloplasty is a surgical procedure to treat ureteropelvic junction (UPJ) obstruction, a blockage that affects urine flow from the kidney to the bladder. It helps prevent kidney damage by restoring normal urine flow. - What causes UPJ obstruction?
UPJ obstruction can be congenital or acquired. It may result from congenital narrowing, scar tissue, kidney stones, or pressure from nearby blood vessels. - What are the benefits of using flap techniques in pyeloplasty?
Flap techniques improve urine flow by creating a wider connection between the renal pelvis and ureter, reducing the risk of re-obstruction and preserving kidney function. - How long is the recovery period after pyeloplasty?
Recovery typically takes about 4-6 weeks. Minimally invasive techniques may allow for faster recovery, while open surgery may require a longer healing time. - Are there any risks associated with pyeloplasty?
Yes, risks include infection, bleeding, stricture formation, leakage, and anesthesia-related complications. However, these risks are relatively low. - Can pyeloplasty be performed laparoscopically or robotically?
Yes, laparoscopic and robotic-assisted pyeloplasty are minimally invasive options that offer quicker recovery, less pain, and smaller incisions than traditional open surgery.