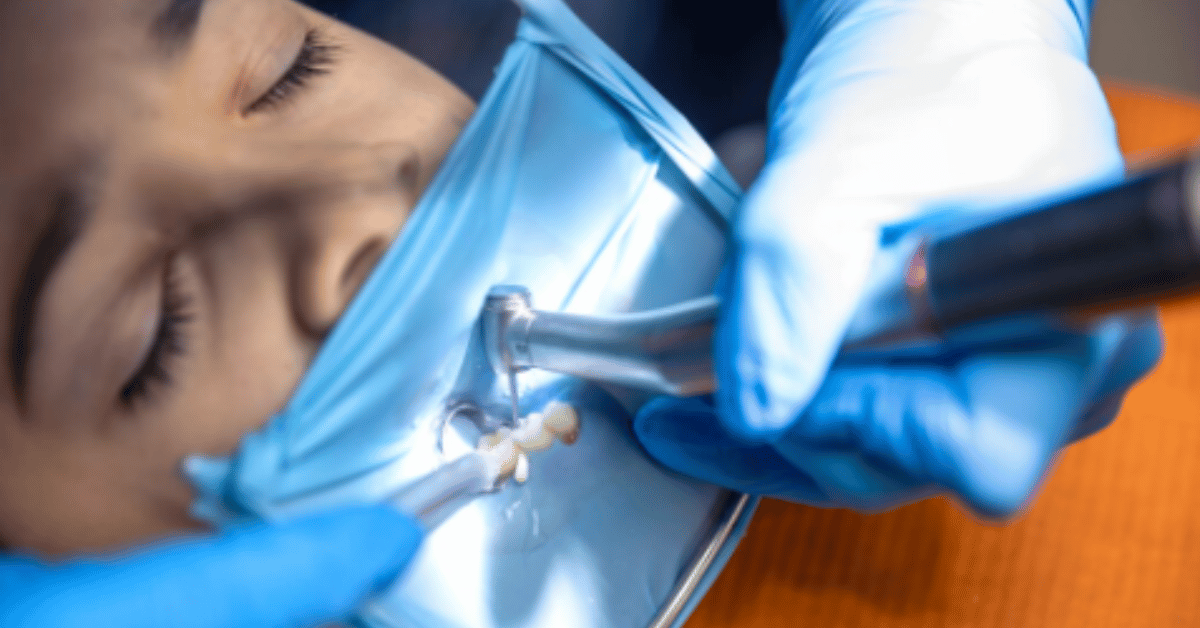
Root canal procedures are often viewed with apprehension due to their association with pain and dental anxiety. For anyone undergoing this procedure, understanding root canal recovery is crucial for effective healing and preventing complications. Within the first 100 words, it’s important to highlight the essential concern of most patients: how to minimize discomfort, manage inflammation, and ensure the treated tooth heals correctly. A root canal removes infected pulp from a tooth’s interior, replacing it with a cleaning and sealing process to preserve tooth function. Recovery isn’t just about managing immediate pain—it’s about long-term oral health, preventing reinfection, and restoring normal chewing and speech functions. Knowledge of post-treatment care, dietary adjustments, and timely follow-ups can significantly improve outcomes, reduce the risk of secondary infection, and support structural integrity of the treated tooth. Root canal recovery is often faster with proper guidance, pain management strategies, and adherence to dentist recommendations.
Recovery time after a root canal varies depending on the tooth treated, the complexity of the infection, and individual health factors. Mild discomfort or soreness typically subsides within two to three days, while more complex cases might take a week or longer. Pain management often involves over-the-counter medications such as ibuprofen or acetaminophen, but severe or persistent pain may require prescription-strength analgesics. Patients are usually advised to avoid chewing on the treated tooth until permanent restoration, like a crown, is placed to prevent fractures. Additionally, swelling and sensitivity can be controlled with cold compresses and proper oral hygiene. Understanding the stages of healing—from initial inflammation to tissue remodeling and full recovery—helps patients anticipate symptoms and know when to contact their dentist. Consistent follow-up visits are critical to ensure the success of the treatment and detect any complications early.
Common Symptoms During Root Canal Recovery
After a root canal, patients may experience various symptoms as part of the natural healing process. Pain or tenderness around the treated tooth is common for the first few days. Swelling in the gums and slight bruising may also occur, which usually decreases over time. Some patients report mild sensitivity to hot or cold foods and beverages. These symptoms are generally temporary and diminish as the tooth stabilizes. However, persistent pain, severe swelling, or pus discharge may indicate an infection or procedural complication, necessitating immediate dental consultation. Patients are advised to maintain meticulous oral hygiene, gently brushing and flossing around the treated area to prevent plaque accumulation and secondary infections. Root canal recovery is supported by avoiding hard, sticky, or extremely hot foods and adhering strictly to dentist instructions regarding medication, diet, and activity restrictions.
| Symptom | Typical Duration | Recommended Action |
|---|---|---|
| Mild pain or soreness | 2–5 days | OTC pain relief, soft diet |
| Swelling | 1–3 days | Cold compress, elevate head |
| Gum bruising | 2–4 days | Gentle oral hygiene |
| Sensitivity to temperature | 1–2 weeks | Avoid extreme temperatures |
| Persistent pain or infection | Beyond 1 week | Contact dentist immediately |
Effective symptom management during the recovery period also includes behavioral adjustments. Patients should avoid smoking and alcohol consumption, which can impair healing. Stress management is important, as stress can affect immune response and delay tissue recovery. Hydration supports overall oral health, and rinsing with saline or mild antiseptic solutions helps prevent bacterial proliferation. Additionally, following any prescribed antibiotics to completion is crucial if the dentist suspects infection risk. Recovery isn’t linear—minor fluctuations in discomfort are normal—but steady improvement should be observed. Tracking symptoms daily and noting any changes ensures timely intervention if complications arise, optimizing both immediate comfort and long-term success of the root canal treatment.
Diet and Lifestyle Adjustments for Faster Recovery
Nutrition plays a critical role in root canal recovery. Immediately after the procedure, patients should consume soft, non-chewy foods like yogurt, mashed potatoes, soups, and smoothies. These foods reduce mechanical stress on the treated tooth while providing essential nutrients to support tissue repair. Avoiding sticky, crunchy, or extremely hard foods minimizes the risk of cracking or dislodging temporary fillings. Patients should also limit acidic foods and beverages, as these can irritate sensitive dental tissues. Incorporating protein-rich foods, leafy greens, and vitamin C-containing fruits supports collagen formation and gum health, while adequate hydration ensures optimal oral tissue function. Long-term dietary adherence, combined with proper dental hygiene, contributes to faster recovery and stronger overall dental resilience.
| Recommended Foods | Foods to Avoid |
|---|---|
| Yogurt | Hard candy |
| Mashed potatoes | Chewing gum |
| Smoothies | Ice cubes |
| Soft cooked vegetables | Crunchy chips |
| Soups | Very hot or acidic drinks |
Lifestyle habits can significantly influence healing outcomes. Avoid excessive physical exertion in the first 24–48 hours to prevent increased blood flow that may exacerbate swelling or bleeding. Elevating the head while resting reduces gum inflammation. Patients are encouraged to practice gentle oral care, avoiding vigorous brushing near the treated area. Consistent follow-ups with the dentist allow monitoring of the restoration process, and timely placement of a crown or filling prevents structural damage. Overall, combining dietary considerations, lifestyle adjustments, and professional guidance ensures a smoother, faster recovery from root canal procedures while minimizing complications and discomfort.
Pain Management Strategies
Pain is often the most concerning aspect of root canal recovery. Fortunately, effective strategies exist to manage post-procedural discomfort. Over-the-counter anti-inflammatory drugs, such as ibuprofen, can reduce swelling and pain. Acetaminophen may be used as an alternative, particularly for patients with gastrointestinal sensitivities. In cases of more severe discomfort, dentists may prescribe stronger analgesics or anti-inflammatory medications. Topical anesthetic gels can provide temporary relief, particularly when brushing near sensitive areas. Applying a cold compress to the affected area for 15–20 minutes at intervals can reduce swelling and discomfort. Patients should avoid excessive chewing and use the treated tooth minimally until permanent restoration. Keeping a pain diary helps patients track the effectiveness of interventions and communicate any unusual symptoms promptly to their dentist.
Other complementary approaches can aid recovery, including relaxation techniques such as deep breathing and meditation to reduce perceived pain intensity. Maintaining adequate hydration supports tissue repair, while avoiding smoking and alcohol consumption prevents delays in healing. Gentle rinsing with warm salt water helps manage gum inflammation and promotes cleanliness around the treated tooth. Pain management is multifaceted and often most effective when combining medications, behavioral strategies, and consistent follow-up with the dental professional. Long-term discomfort beyond the typical recovery window may indicate procedural complications or reinfection, emphasizing the importance of timely evaluation and intervention.
Oral Hygiene and Care During Recovery
Maintaining proper oral hygiene is vital to ensure successful root canal recovery. While the treated area may be tender, brushing gently with a soft-bristled toothbrush is recommended. Flossing should continue but with extra care to avoid disturbing temporary fillings or causing tissue trauma. Antiseptic mouthwashes can reduce bacterial load and support gum health. Avoid aggressive rinsing or using water picks directly on the treated tooth in the first few days. Regular dental check-ups are crucial to monitor healing, assess tissue response, and determine when permanent restoration is appropriate. Patients who follow these hygiene practices reduce the likelihood of reinfection, swelling, or prolonged sensitivity. “Oral hygiene is not just about cleaning—it is integral to the success of restorative dental procedures,” says Dr. Karen Reynolds, a practicing endodontist.
Patients should be aware that even minor lapses in hygiene can compromise recovery. Neglecting care around the treated tooth can lead to plaque accumulation, bacterial invasion, and secondary infection, which may necessitate retreatment. Using fluoride toothpaste strengthens tooth enamel, while gentle massage of surrounding gums promotes blood flow and healing. Monitoring for unusual signs, such as persistent bleeding or pus formation, allows early intervention. Adhering to dentist recommendations regarding brushing technique, mouthwash use, and follow-up appointments maximizes the longevity of the root canal treatment and minimizes potential complications. Long-term dental health benefits greatly from consistent and careful oral care during this critical recovery period.
Recovery Timeline and Stages
The timeline for root canal recovery varies but generally follows a predictable pattern. Immediately after the procedure, patients may experience mild discomfort, swelling, or gum sensitivity. The first 48–72 hours typically see the most noticeable pain and inflammation, which should gradually decline. By the end of the first week, most patients experience significantly reduced discomfort, and normal oral function begins to return. Complete tissue healing and full integration of the treated tooth may take several weeks, depending on the tooth type and individual health. Follow-up appointments during this period ensure the tooth is healing properly and allow the dentist to place permanent restorative materials. Understanding these stages helps patients manage expectations and adhere to care recommendations for optimal outcomes.
| Recovery Stage | Duration | Key Indicators |
|---|---|---|
| Immediate post-procedure | 0–48 hours | Soreness, mild swelling, gum tenderness |
| Early recovery | 3–7 days | Decreasing pain, mild sensitivity |
| Intermediate recovery | 1–3 weeks | Normal function returns, tenderness fades |
| Complete recovery | 3–6 weeks | Full tissue healing, permanent restoration placement |
Adherence to recovery timelines supports better planning for professional follow-ups and minimizes the risk of complications. Knowing what to expect reduces patient anxiety and encourages proactive care. Patients should maintain communication with their dentist, reporting any persistent or worsening symptoms. Recovery may be influenced by pre-existing dental conditions, the complexity of the root canal procedure, and overall health. Maintaining a structured care plan, including pain management, diet adjustments, oral hygiene, and timely professional evaluations, ensures the treated tooth remains functional, infection-free, and structurally sound for years to come.
FAQs
1. How long does it take to fully recover from a root canal?
Full recovery generally takes between three to six weeks, though most patients notice significant improvement within the first week. Immediate post-procedure soreness or mild swelling usually lasts 2–5 days. Recovery speed depends on factors such as the complexity of the treated tooth, pre-existing dental infections, overall health, and adherence to post-procedure instructions. Early follow-ups and proper oral hygiene are crucial to ensuring complete healing and preventing reinfection. “Recovery timelines vary, but patients who follow care instructions experience smoother and faster healing,” notes Dr. Laura Chen, an endodontist with 15 years of experience.
2. Is it normal to feel pain after a root canal?
Yes, mild pain or tenderness is normal for several days after a procedure. The tooth may feel sensitive to biting or pressure. Over-the-counter pain relievers such as ibuprofen or acetaminophen are usually sufficient, though your dentist may prescribe stronger medication for more complex cases. Persistent or worsening pain, swelling, or pus may indicate infection or complications, requiring prompt professional evaluation.
3. Can I eat normally after a root canal?
Immediately after the procedure, patients should eat soft, non-chewy foods to avoid stress on the treated tooth. Smoothies, yogurt, soups, mashed vegetables, and soft proteins are ideal. Avoid sticky, crunchy, or hard foods until the permanent restoration, like a crown, is placed. Maintaining proper nutrition supports tissue repair and accelerates recovery while minimizing the risk of tooth fracture.
4. How should I care for my tooth during recovery?
Gentle oral hygiene is essential. Brush with a soft-bristled toothbrush, floss carefully around the treated area, and use antiseptic mouthwash if recommended. Avoid aggressive rinsing or water picks directly on the treated tooth for the first few days. Regular dental follow-ups ensure proper healing and timely placement of permanent restorations.
5. What are the signs of complications?
Watch for severe or worsening pain, prolonged swelling, pus discharge, persistent bleeding, or fever. These signs may indicate infection or treatment failure. Prompt contact with your dentist ensures timely intervention, preventing further damage or retreatment.