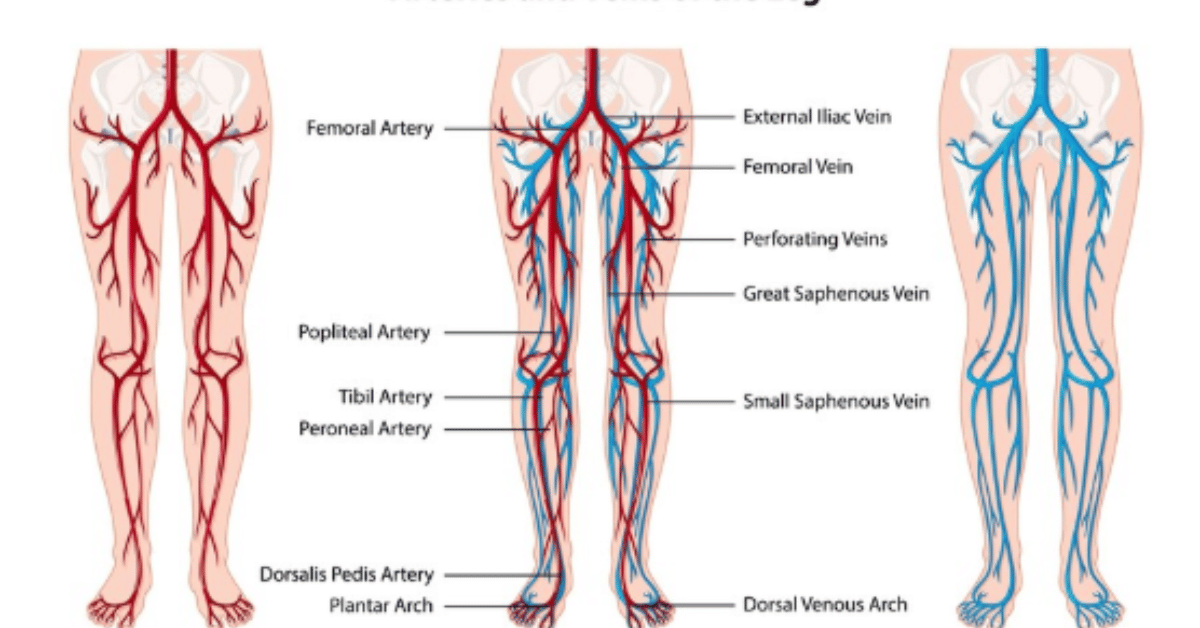
If you’ve ever been scheduled for a vein procedure—be it dialysis access, varicose vein treatment, or bypass surgery—you’ve likely heard of “vein mapping.” But what exactly is it, why is it performed, and what can it reveal? In essence, vein mapping is a non-invasive diagnostic ultrasound technique used to visualize the veins beneath the skin, especially in the arms and legs. Its goal is to identify suitable veins for medical procedures or to assess vascular health. While simple in concept, its implications are broad, influencing treatment outcomes and patient safety across multiple specialties.
Table: Overview of Vein Mapping Insights
| Aspect | Details |
|---|---|
| Purpose | Locate healthy, usable veins for surgery, dialysis, or treatment |
| Technology Used | Duplex ultrasound (combines soundwaves with Doppler imaging) |
| Typical Candidates | Dialysis patients, varicose vein sufferers, those needing bypass surgery |
| Time Required | Usually 30 to 60 minutes |
| Pain Level | Non-invasive and painless |
| Results | Real-time images and flow data for clinical decisions |
| Post-Mapping Use | Surgical planning, access placement, vascular assessments |
The Origins and Rise of Vein Mapping
Originally a tool confined to vascular surgery, vein mapping has steadily evolved into a common diagnostic procedure in hospitals and outpatient clinics alike. Initially, surgeons sought precise ways to find appropriate veins for coronary artery bypass grafting. As ultrasound technology advanced, clinicians realized its utility could expand—especially in nephrology and interventional radiology.
What makes vein mapping uniquely valuable is its ability to provide both anatomical and functional data. This dual capability means clinicians are not merely seeing where the veins are, but also how well they perform under stress.
Who Needs Vein Mapping and Why?
1. Dialysis Access Planning
One of the most critical uses of vein mapping is in patients requiring hemodialysis. These patients need an arteriovenous (AV) fistula or graft—surgically connecting a vein to an artery. Vein mapping ensures the selected vein is healthy enough to support repeated access.
2. Varicose Vein Treatment
For patients with chronic venous insufficiency or varicose veins, vein mapping helps determine which veins are functioning improperly. By understanding where valves fail and where reflux occurs, doctors can create a treatment roadmap—laser ablation, sclerotherapy, or stripping.
3. Coronary Artery Bypass Surgery (CABG)
In cardiac surgery, the saphenous vein from the leg is often used as a bypass graft. Mapping ensures that the vein is long enough and free of thrombosis or other issues.
4. Peripheral Arterial Disease (PAD)
In PAD cases, when leg arteries are blocked, vein mapping helps determine whether autologous veins can be used for bypass.
5. Trauma and Emergency Vascular Access
In emergent settings where IV access is difficult, vein mapping assists in locating suitable large veins.
The Procedure: What to Expect
Vein mapping’s relatively simple, outpatient-based, and non-invasive. Here’s how the process typically unfolds:
Pre-Procedure
- No fasting or medication restrictions
- Patient wears loose-fitting clothing
- Brief history and consent obtained
During the Scan
- Patient lies flat or sits upright, depending on area being mapped
- A warm gel is applied to the skin to aid soundwave transmission
- A transducer (ultrasound probe) is moved over the skin to capture images
- The technician measures diameter, compressibility, depth, and valve function
Post-Procedure
- Gel is wiped off
- Results are interpreted by a radiologist or vascular surgeon
- Reports and annotated images are delivered to the referring physician
Key Parameters Evaluated in Vein Mapping
| Parameter | Clinical Relevance |
|---|---|
| Diameter | Minimum required size for dialysis fistula or graft |
| Depth | Affects surgical accessibility |
| Compressibility | Indicates clot presence or chronic damage |
| Valve Competency | Important for treating varicose veins |
| Flow Rate | Helps assess the ability to support access or bypass |
Advancements in Vein Mapping: What’s New?
In recent years, innovations have changed how vein mapping’s performed and interpreted.
High-Frequency Transducers
Modern transducers with higher frequencies deliver sharper, more detailed images of superficial veins, which is critical when evaluating small veins for pediatric or elderly patients.
AI-Augmented Analysis
Some centers are implementing machine learning algorithms that auto-analyze vein structure and flow patterns, reducing technician variability.
Portable Mapping
With handheld ultrasound devices, vein mappings can now be performed bedside—even in rural clinics or home-care setups—bringing the technology closer to patients.
Misconceptions About Vein Mapping
1. “It’s Only for Surgery.”
False. Vein mapping’s useful in chronic conditions, cosmetic assessments, and even sports medicine when repetitive use affects vascular structures.
2. “It’s a Treatment.”
No—it’s a diagnostic tool. It identifies the problem; it doesn’t fix it.
3. “It Always Leads to Surgery.”
Often, vein mappings rules out surgery by offering conservative management options, such as compression therapy or medication.
Case Study: Dialysis Patient and Mapping Impact
Patient: 58-year-old male with end-stage renal disease
Challenge: Scarred veins from prior IV drug use
Outcome: Vein mappings identified a single viable basilic veins. A successful transposition surgery created a durable AV fistula.
Without mapping, the surgical attempt may have failed, risking patient health and increasing healthcare costs.
The Cost and Accessibility of Vein Mapping
Vein mapping costs vary by location and insurance coverage but typically range from $200 to $800. Most public and private insurance plans cover it when medically necessary.
As technology becomes more portable and accessible, many rural clinics are adopting handheld devices, ensuring equitable diagnostic access.
Risks and Safety Profile
Vein mapping’s safe for nearly all patients. There’s no exposure to radiation or injections. Rarely, minor discomfort from prolonged probe pressure occurs, but this resolves immediately.
Importance for Personalized Medicine
Vein mappings embodies the move toward individualized care. Not all patients have textbook anatomy, and what works for one patient may not work for another. By revealing a person’s unique vascular “fingerprint,” clinicians can plan precisely, reducing risks and improving outcomes.
When Should You Ask About Vein Mapping?
You should request or inquire about vein mappings if:
- You are preparing for dialysis access
- You’ve been advised to undergo a vein-related surgery
- You’ve had failed previous vascular procedures
- You are exploring treatment for varicose or spider veins
- You are undergoing chemotherapy and have difficult IV access
Future of Vein Mapping
Looking forward, vein mapping’s poised to become even more precise:
- 3D vascular modeling for pre-surgical simulation
- Tele-ultrasound where technicians guide remote providers via live video
- Integration with EHRs for real-time clinical decision-making
Summary: Why Vein Mapping Matters
Vein mappings may not be flashy, but its clinical value is undeniable. It prevents surgical complications, guides treatment decisions, and customizes care. In a healthcare landscape shifting rapidly toward efficiency and accuracy, this non-invasive technique stands at the intersection of old-fashioned diagnostics and next-generation care.
FAQs
Q1: Is vein mapping painful?
No, it’s completely non-invasive and painless, involving only ultrasound gel and light probe contact.
Q2: How long do results take?
Usually same-day results or within 24 hours, depending on facility and urgency.
Q3: Do I need to prepare in any special way?
No special prep is needed. Loose clothes help, especially if mapping arms or legs.
Q4: Can vein mapping detect blood clots?
Yes, it can identify clots, but a full DVT scan may be ordered if clots are suspected.
Q5: Is this covered by insurance?
Most insurance plans cover vein mapping when it’s ordered for a medical reason.